
The Opioid Crisis Initiative
According to the US Centers for Disease Control and Prevention, more than 750,000 people have died since 1999 from a drug overdose. More than two out of three drug overdose deaths in 2018 involved an opioid. Opioids are substances that work in the nervous system of the body or in specific receptors in the brain to reduce the intensity of pain. They are known to be one of the most addictive medicines for thousands of years. Overdose deaths involving opioids, including prescription opioids, heroin, and synthetic opioids (like fentanyl), have increased almost six-fold since 1999.
In 2018, 67,367 drug overdose deaths occurred in the United States. Overdoses involving opioids killed nearly 47,000 people in 2018, and 32% of those deaths involved prescription opioids. This means that opioids were responsible for nearly 70% of all overdoses in 2018 and that most of these deaths are avoidable with appropriate care and education.
The primary initiative of the Board of Medicine is to provide harm-reduction for those dependent on opioids and other prescription medicines with similar addictive potential (benzodiazepines, barbiturates, sedatives, hypnotics, and stimulants). The purpose of the Board of Medicine’s Opioid Crisis Initiative is to provide risk-free non-addictive alternatives for those in desperate need of solutions.
There are many healthy options for those struggling with opioid dependence. There is strong evidence for numerous plant medicines, psychotherapy techniques, cannabinoids, and some new wearable technologies that demonstrate promising results from ongoing studies. All of these alternatives are considered to have a negligible risk of dependence and few to no adverse effects, which automatically makes them attractive as tools to tackle the opioid crisis.
As an example, In one JAMA article reviewed by Dr. Peter Grinspoon MD for Harvard Medical School published by Harvard Health Publishing, a longitudinal analysis of the number of opioid prescriptions filled under Medicare Part D, showed that when medical marijuana laws went into effect in a given state, opioid prescriptions fell by 2.21 million daily doses filled per year. When medical marijuana dispensaries opened, prescriptions for opioids fell by 3.74 million daily doses per year. These reductions in daily opioid doses were particularly notable for hydrocodone (Vicodin) and morphine prescriptions, but these dosing reductions also extended to benzodiazepines, stimulants, and many mental health medications that are known to be over-prescribed. This was discussed in a timely 2017 article by Dr. Yasmin Hurd in depth.
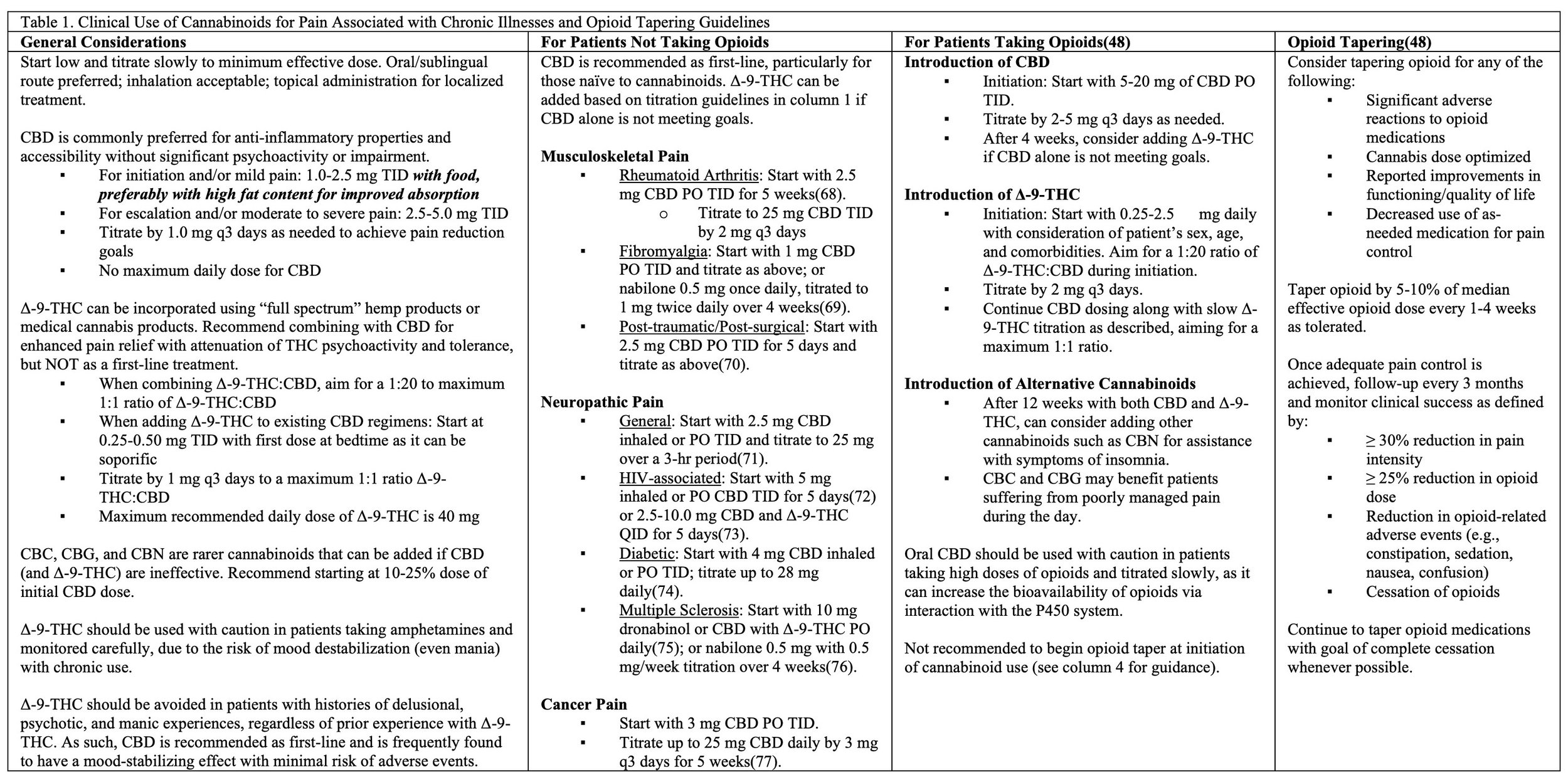
In 2023, the Board of Medicine team published some of the world’s first comprehensive clinical guidelines recommending evidence-based treatment programs for improving harm-reduction when managing opioid dependence and chronic pain using cannabinoids entitled: An answered call for aid? Cannabinoid clinical framework for the opioid epidemic
To stay up to date on our clinical guidelines and trainings, please send us your contact information using the short form at the bottom of the page.
Contact us.
Please reach out to us to get involved with the Board, sign up for our trainings, and stay up to date on our latest developments.
info@theboardofmedicine.org
